“While many Americans share those concerns, polls show that large majorities of Americans – Democrats, Republicans and Independents – have consistently supported government negotiation of drug prices.
“Most Democrats and patient groups have pushed for changes to the law that would allow the government to negotiate prices through Medicare under a cap pegged to what other wealthy nations pay.
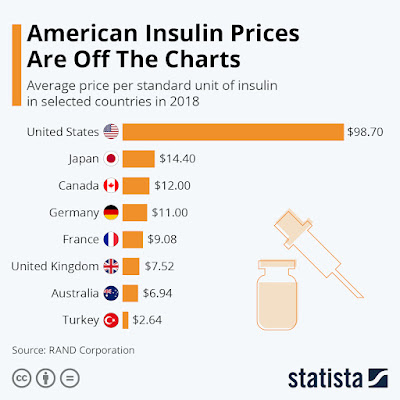
"'The United States is alone among developed countries in not having a role for the government in negotiating or setting the price of drugs, and that's why we pay much higher prices than the rest of the world,' said Larry Levitt, executive vice president for health policy at the nonpartisan Kaiser Family Foundation.
“Levitt continues: 'The idea is not just to have Medicare negotiate prices for its own program but to extend those negotiated prices to private insurance plans as well, This would put drugs on equal footing with other types of health care. Medicare negotiates or sets the price for hospital care, for doctor visits.'"
(Devin Dwyer, Erica Y King, and Trish Turner. “Prescription drug cost relief nixed from Democrats' plan.” ABC News. October 28, 2021.)
The federal government could save $450 billion over 10 years, according to one Congressional Budget Office analysis -- savings that could help offset the costs of other initiatives or reduce the deficit. Consumers would also reap savings at the pharmacy counter.
However …
Drug companies have warned that the trade-offs from lost revenue would be significant, upending a key part of the U.S. economy, leading to job losses and less money for research and development of new drugs.
"Of course we make profit, but it's not like we keep it, right? We return it to shareholders who give us money to take huge risk on R&D," said Lilly CEO Dave Ricks, whom public filings show received a $23 million compensation package last year.
ABC News reports that Ricks estimates that despite earning billions in profits, the company would have to cut experimental drug projects in half if the government capped prices – curbing the kind of innovation seen from manufacturers during the COVID-19 pandemic.
An independent government analysis forecasts there would be two fewer new drugs brought to market over the next 10 years, with 23 fewer over the decade after that.
So …
The White House on Thursday said the idea doesn't have enough votes in Congress to support government negotiation of drug prices.
"At the end of the day, there are not yet enough votes to get something across the line," a senior Biden administration official, who asked not to be identified, told reporters.
Sen. Ron Wyden, D-Oreg., who chairs the Senate Finance Committee and is a leading advocate for Medicare drug negotiations, says he is still fighting for a slimmed-down version of the plan.
Sen. Bernie Sanders, I-Vt., is also adamant that the proposal be restored before a final vote on the social spending plan.
"The American people are very, very clear that they are sick and tired of paying the highest prices in the world for prescription drugs," he said. "It is really outrageous that year after year, members of Congress talk about the high cost of prescription drugs and yet, year after year, we are not able to do anything about it."
(Devin Dwyer, Erica Y King, and Trish Turner. “Prescription drug cost relief nixed from Democrats' plan.” ABC News. October 28, 2021.)
There We Go Again
Everyone understands the exorbitant profit made by drug companies.
Researchers writing in the Journal of the American Medical Association (JAMA) investigated the financial balances of pharma companies dealing in the business of developing, manufacturing, marketing and selling drugs.
(Fred D. Ledley, Sarah Shonka McCoy, Gregory Vaughan, Ekaterina Galkina Cleary. “Profitability of Large Pharmaceutical Companies Compared With Other Large Public Companies. JAMA. 2020 Mar 3; 323(9): 834–843.)
Their calculations found that in the years between 2000 and 2018, 35 big drug companies received a combined revenue of $11.5 trillion, with a gross profit of $8.6 trillion.
In comparison, the study authors, who are associated with Bentley University in Waltham, Mass., point out that during the same time period, 357 S&P 500-traded companies reported cumulative revenue of $130.5 trillion, gross profit of $42.1 trillion, EBITDA of $22.8 trillion and net income of $9.4 trillion.
However, when looking at bivariable regression models, the researchers found that the median annual profit margins of pharmaceutical companies were significantly greater than those of S&P 500 companies. They found that a 39.1% difference in gross profit margin, 76.5% for pharma companies and 37.4% for the S&P companies.
Richared Frank and Paul Ginsburg in Health Affairs, a publication of Project HOPE, consider if the yield from additional resources going into research and development justify what society is paying in the form of higher prices for drugs?…
“Over-investment in certain clinical areas is driven by competition. And, in a market economy, with government acting only to provide patent protection and exclusivity to allow innovation to be viable, drug prices are set by supply and demand.
“Since much of the cost of producing drugs involves the research and development to create them – as opposed to the cost of manufacturing the pills – the price that can be obtained influences the amount that is invested in development of new drugs. However on the demand side, higher prices lead to fewer units of the drug being sold.
“This demand constraint leads to investment being sensitive to value – what a drug accomplishes medically for patients compared to what it will cost. To the degree that health insurance pays for a substantial portion of the price of drugs, manufacturers can charge higher prices and likely will invest more to develop new drugs.
(Richard G. Frank and Paul B. Ginsburg. “Pharmaceutical Industry Profits And Research And Development.” Health Affairs. November 13, 2017.)
High Prices Without Negotiation
The development – lack of votes in Congress – dashed hopes for what many consumer advocates had considered the best chance in decades for immediate relief to families burdened by soaring costs of medication.
A popular plan to let the government directly negotiate lower prescription drug prices with pharmaceutical companies – extracting significant savings for taxpayers and patients – will likely not be part of the Democrats' sweeping social spending package, the White House said..
It also marks a major victory for drug makers who have spent millions of dollars lobbying against direct government intervention in pricing.
A Tale of Insulin: Life and Death
The most commonly used forms of analog insulin cost 10 times more in the United States than in any other developed country.
(Emily Rauhala. “American diabetics are crossing borders into Canada in order to get life-saving insulin.” Independent. July 01, 2019.)
Annual insulin costs doubled between 2012 and 2016, a fact with a death toll attached to it. There’s no single force propelling insulin prices to newly dangerous heights, but the problem is exacerbated by the flaws of America’s heavily privatized health-care system.
A lengthy piece in the Washington Post Magazine suggested that pharmaceutical companies and pharmacy benefit managers (PBMs) like CVS Health share the blame. The pharmaceutical companies have raised prices in near lockstep.
“Every time a PBM extracts a deeper discount, an insulin manufacturer has the incentive to take a price increase to quote ‘make themselves whole,’” health economist Rena Conti told the Post.
(Tiffany Stanley. “Life, Death, and Insulin.” The Washington Post Magazine. January 07, 2021.)
As insulin prices rise, patients go without. One study in the Journal of the American Medical Association, cited by the Guardian, found that around one in four patients with diabetes say they ration the medicine due to cost, but pharmaceutical companies show little interest in slashing prices back down to humane levels. Meanwhile, rationing can have dangerous consequences for patients who depend on insulin to survive.
A 2019 study by the Centers for Disease Control and Prevention found that almost 1 in 7 of U.S. adults with diabetes weren’t using insulin as prescribed by their doctors because of the high cost.
There have been many recent reports of deaths in patients with type 1 diabetes because of lack of affordable insulin. The high prevalence of diabetes, the chronic lifelong nature of the disease, and the fact that patients with type 1 diabetes will die without access to insulin make this an urgent problem that must be solved expeditiously. The price of insulin is also a stark and troubling example of the rising cost of prescription drugs in the United States and highlights a systemic problem with how drugs are priced compared with every other commodity.
(S. Vincent Rajkumar, MD. “The High Cost of Insulin in the United States: An Urgent Call to Action.” Mayo Clinic Proceedings. Volume 95, issue 1, January 01, 2020.)
The Mayo Clinic Proceedings reports ...
“The 3 main reasons cited by pharmaceutical companies for the high cost of new prescription drugs do not apply to insulin. First, the “high cost of development” is not relevant for a drug that is more than 100 years old; even the latest and most commonly used analog insulin products are all over 20 years old.
“Second, the pricing is not the product of a free market economy. Free market forces are clearly not operational; there is limited competition on price, the person who needs the product is not in a position to negotiate the price, and there is no relationship of price increases over time compared with overall market inflation. The price of insulin has risen inexplicably over the past 20 years at a rate far higher than the rate of inflation.
“One vial of Humalog (insulin lispro), which used to cost $21 in 1999, costs $332 in 2019, reflecting a price increase of more than 1000%.
“In contrast, insulin prices in other developed countries, including neighboring Canada, have stayed the same. Insulin pricing in the United States is the consequence of the exact opposite of a free market: extended monopoly on a lifesaving product in which prices can be increased at will, taking advantage of regulatory and legal restrictions on market entry and importation. Third, the arguments that high costs are needed for continued innovation and that attempts to lower or regulate the prices will hamper innovation are not a valid excuse.
“There is limited innovation when it comes to insulin; the more pressing need is affordability.”
(S. Vincent Rajkumar, MD. “The High Cost of Insulin in the United States: An Urgent Call to Action.” Mayo Clinic Proceedings. Volume 95, issue 1, January 01, 2020.)
Mayo cites the number 1 reason for the high cost of insulin is the presence of a vulnerable population that needs insulin to survive. This population, which numbers in the millions is willing to pay anything to have access to a lifesaving drug. The desperate need for a lifesaving product allows insulin to be priced at high levels because it is not a luxury item that one can forego. The manufacturers of insulin know that patients who need it will spend whatever it takes to acquire it, regardless of price. It is a matter of life and death.
Mayo concludes …
“The tragedy of insulin prices and the rationing that follows is not something that happens in other developed countries, but it is common in the United States. A study conducted at Yale University found that 25% of patients with diabetes ration insulin because of the high cost. There are 30 million patients with diabetes in the United States, and approximately 25% (7.4 million Americans) need insulin. For the 1.3 million patients with type 1 diabetes, insulin is as vital as air and water. We cannot wait to act.”
(S. Vincent Rajkumar, MD. “The High Cost of Insulin in the United States: An Urgent Call to Action.” Mayo Clinic Proceedings. Volume 95, issue 1, January 01, 2020.)
Conclusions
Why does it seem so often the most basic human needs are denied by the government in favor of corporate profit and greed? Human rights exist independent of our culture, religion, race, nationality, economic status … or political party.
I share the views of Mary Gerisch, a board member of the National Center for Law and Economic Justice. Gerisch reminds us …
“Through the free exercise of those rights can we enjoy a life of dignity. Universal health care is crucial to the ability of the most marginalized segments of any population to live lives of dignity.
“Therefore, we must name and claim our right to health. Only then can we tip the balance of power to demand our government institute a true and universal health care system. In a country with some of the best medical research, technology, and practitioners, people should not have to die for lack of health care including the lack of essential drugs.
“The real meaning of this right to health care requires that all of us, acting together as a community and society, take responsibility to ensure that each person can exercise this right. As individuals, we have a responsibility to contribute to making health care available to each of us.”
(Mary Gerisch, “Health Care As a Human Right.” American Bar Association. Vol. 43, No. 3: The State of Healthcare in the United States.)


No comments:
Post a Comment